Numerous books explore the psychology of chronic pain, addressing the intersection of mental and physical factors. Key themes include:
- Cognitive-Behavioral Therapy (CBT) for cognitive distortions.
- Acceptance and Commitment Therapy (ACT) promoting psychological flexibility.
- Mindfulness-based interventions enhancing coping mechanisms.
Research supports these treatment methods, emphasizing their effectiveness on pain management. Additionally, social factors and cultural influences play significant roles in pain perception. Understanding these dimensions is essential for effective pain management. Further exploration reveals additional insights.
Key Takeaways
- “The Mindful Way Through Pain” emphasizes mindfulness techniques to differentiate physical pain from emotional suffering and promote coping strategies.
- “Healing Back Pain” by John Sarno explores the psychological causes of chronic pain and how emotional awareness can alleviate symptoms.
- “The Pain Management Workbook” provides practical exercises grounded in cognitive-behavioral therapy to address maladaptive thoughts related to pain.
- “The Body Keeps the Score” by Bessel van der Kolk discusses the interplay between trauma, psychology, and chronic pain, highlighting the importance of emotional expression.
- “Acceptance and Commitment Therapy for Chronic Pain” offers insights into how acceptance strategies can improve psychological flexibility and enhance quality of life.
Overview of Psychological Treatments for Chronic Pain
Psychological treatments for chronic pain represent a crucial component of thorough pain management strategies. Cognitive-Behavioral Therapy (CBT) is the most commonly used approach, targeting cognitive distortions that contribute to distress and maladaptive behaviors, such as social withdrawal.
Key components of CBT include:
- Teaching behavioral coping skills, including relaxation techniques.
- Proven effectiveness in reducing pain severity, disability, and emotional distress in multiple trials.
Mindfulness-based interventions also play an essential role, promoting present-moment awareness to differentiate physical pain from emotional suffering. These techniques encourage non-judgmental observation of pain, enhancing emotional processing and regulation.
Emotional-Awareness and Expression Therapy addresses the connection between emotions and pain, facilitating the expression of suppressed feelings to alleviate pain symptoms. Together, these modalities foster thorough pain management.
Acceptance and Commitment Therapy (ACT) Explained

Acceptance and Commitment Therapy (ACT) represents a progressive approach in the treatment of chronic pain, building on the foundation established by Cognitive-Behavioral Therapy.
Core Principles
- ACT emphasizes acceptance strategies, guiding individuals to acknowledge pain as part of their experience rather than an adversary.
- Mindfulness techniques enhance present-moment awareness, reducing emotional distress linked to pain.
Behavioral Commitment
- Commitment techniques focus on aligning actions with personal values, encouraging patients to engage in meaningful activities despite pain.
- This therapy aims to foster psychological flexibility, enhancing coping mechanisms and empowering patients to take control of their lives.
Clinical Evidence
– Research supports ACT’s efficacy in improving function and quality of life among chronic pain populations, making it a valuable component of thorough pain management strategies.
Neuroscience Insights Into Chronic Pain
Chronic pain is a multifaceted condition rooted in complex neurobiological processes, which can markedly affect an individual’s quality of life.
Neural Correlates and Pain Pathways****
- Central sensitization contributes to heightened sensitivity in the nervous system, resulting in persistent pain from both noxious and innocuous stimuli.
- Altered receptor activity, particularly of ionotropic glutamate receptors, enhances excitatory neurotransmission within pain pathways.
Neuroplastic Changes
- Chronic pain induces neuroplastic changes, impacting the spinal cord, brainstem, and vagus nerve, which can exacerbate pain responses.
- Disruption in potassium-chloride cotransporter function leads to increased excitability in dorsal horn neurons.
Chronicity Mechanisms
– These mechanisms sustain pain chronification, influencing both sensory processing and emotional dimensions of the pain experience.
Mind-Body Perspectives on Pain Management

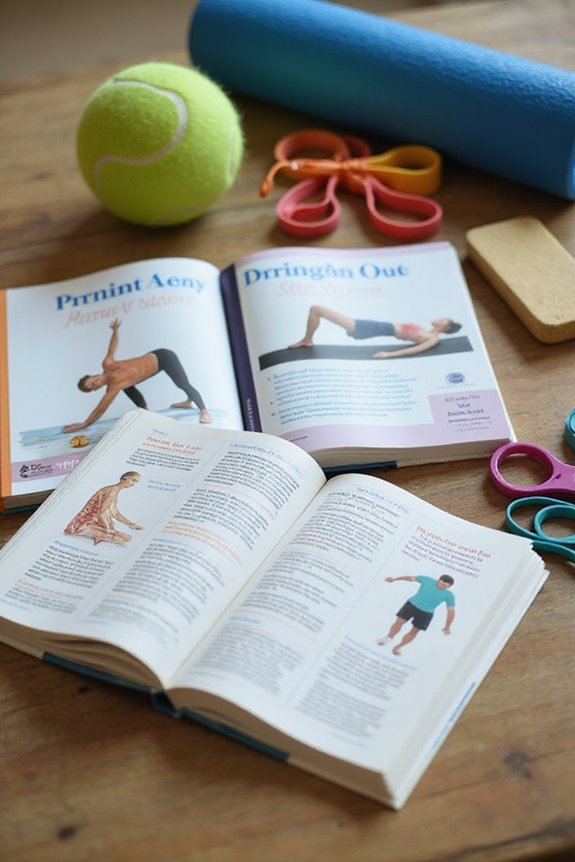
Mind-body therapies are increasingly recognized as essential components in the management of pain, integrating psychological and physiological strategies to enhance patient outcomes. These approaches include:
- Somatic Therapies: Techniques like yoga and Tai Chi promote physical movement and relaxation, addressing both pain and emotional resilience.
- Mindfulness-Based Stress Reduction (MBSR): This method fosters awareness of pain, reducing distress and enhancing coping mechanisms.
- Cognitive-Behavioral Therapy (CBT): CBT targets maladaptive thoughts, improving pain management effectiveness.
Research indicates these therapies can considerably reduce pain intensity and improve physical function. Additionally, they may decrease reliance on opioid medications. By addressing the interplay between mind and body, these therapies offer a holistic approach to chronic pain management, promoting overall well-being.
Self-Management Strategies for Chronic Pain

Self-management strategies for pain are essential in empowering individuals to take an active role in their treatment. These strategies encompass various self management techniques and coping strategies that enhance understanding and control over chronic pain.
- Educational interventions increase awareness of pain mechanisms, promoting symptom monitoring and treatment adherence.
- Peer support in group settings fosters shared experiences, reducing isolation and enhancing motivation.
- Incorporating physical activity and pacing techniques counters deconditioning and improves daily functioning.
- Cognitive-Behavioral Therapy (CBT) offers tools for cognitive restructuring and relaxation, addressing maladaptive thoughts.
- Skill development programs focus on monitoring triggers, goal setting, and problem-solving to enhance self-efficacy.
Incorporating these methods can greatly improve the quality of life for those managing chronic pain.
The Role of Mindfulness in Pain Relief
While pain management remains a critical aspect of healthcare, mindfulness has emerged as a promising approach for alleviating pain symptoms.
- Mindfulness meditation fosters purposeful, present-moment awareness, which can enhance emotional regulation.
- Research indicates that mindfulness reduces pain intensity and unpleasantness by modulating specific brain regions involved in cognitive control and emotional response, such as the orbitofrontal cortex and anterior insula.
- Studies show significant reductions in pain unpleasantness ratings following mindfulness interventions, particularly in experienced meditators.
- This technique not only helps separate pain from self-identity but also diminishes negative emotional reactions associated with pain.
- Importantly, mindfulness engages mechanisms independent of opioid neurotransmission, offering a non-pharmacological alternative for chronic pain relief.
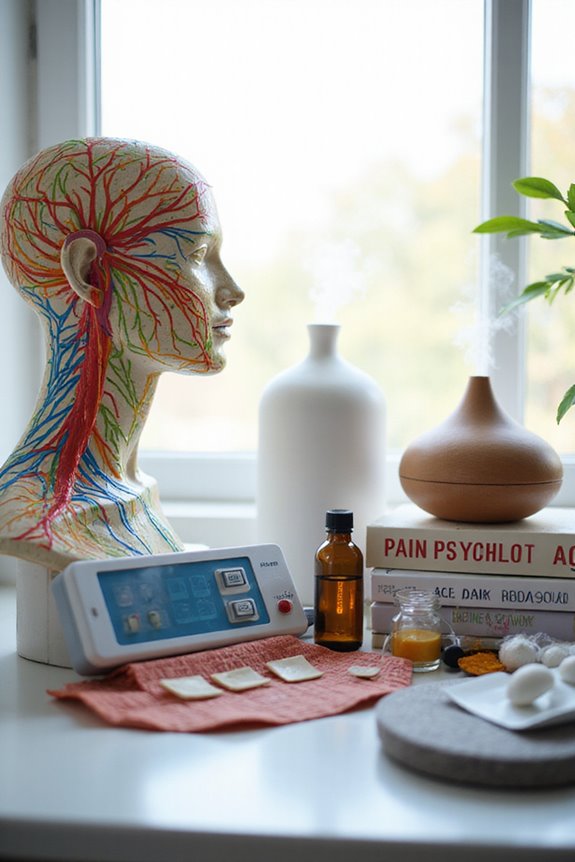
Complementary Techniques for Managing Pain
Complementary techniques for managing pain offer additional avenues for individuals seeking relief beyond conventional medical treatments.
Acupuncture Benefits
This ancient practice stimulates the nervous system and promotes healing, potentially easing chronic conditions like back pain and migraines.
Massage Techniques
Manipulation of soft tissues enhances blood flow and reduces stress, providing immediate relief for various pain conditions.
Biofeedback Applications
This non-invasive method teaches control over physiological responses, helping to reduce tension and improve symptoms in conditions like tension headaches.
Cannabis Safety
Medical cannabis may aid in managing chronic pain but requires supervision due to potential side effects.
Guided Imagery
Visualization techniques can shift focus away from pain, promoting relaxation and potentially reducing perceived pain intensity. Infrared light therapy has also shown promise in enhancing healing and reducing inflammation, offering an additional complementary approach.
Cultural Influences on Pain Perception
Cultural influences greatly shape pain perception, impacting how individuals experience and communicate their discomfort.
- Cultural background alters pain definitions, with some viewing it as a medical issue, while others see it as a spiritual test.
- Attitudes towards pain communication differ; for example, Asian cultures may exhibit stoicism, necessitating reliance on non-verbal cues for assessment.
- In some communities, collective well-being takes precedence over individual pain expression, affecting reporting.
- Cultural perceptions also influence opioid acceptance, with fears of addiction complicating treatment for African American patients.
- Additionally, cultural competence among healthcare providers is essential; misinterpretation of pain communication can lead to inadequate care.
Understanding these factors is vital in addressing healthcare disparities and improving pain management across diverse populations.
Social Dimensions of Chronic Pain Psychology
The experience of chronic pain is markedly influenced by social dimensions, which encompass the interplay of relationships, community involvement, and emotional support.
- Strong social support correlates with reduced emotional distress, enhancing pain management outcomes.
- Conversely, limited social support exacerbates feelings of loneliness and intensifies pain perception.
- Individuals with chronic pain often experience social isolation, leading to dissatisfaction in social roles and higher emotional distress levels.
- Group-based interventions can enhance social support networks, improving pain-related symptoms.
- Disparities in access to social support exist across demographic groups, further complicating chronic pain experiences.
- Understanding the nuances of social dynamics is essential for effective pain management, as emotional distress is deeply intertwined with the social environment.
Frequently Asked Questions
How Can Chronic Pain Affect Relationships and Social Interactions?
How does chronic pain create communication barriers that deepen emotional distance? This condition strains relationships, leading to social withdrawal and reduced intimacy, ultimately challenging the bonds that foster belonging and support within couples and their wider social networks.
What Role Does Nutrition Play in Managing Chronic Pain?
Nutrition strategies and dietary supplements play essential roles in managing chronic pain, enhancing overall well-being. By promoting anti-inflammatory effects and improving nutrient intake, individuals can experience reduced pain severity and improved quality of life, fostering community support.
Are There Specific Self-Help Books for Chronic Pain Sufferers?
In the domain of chronic pain, self-help books offer strategies for empowerment, juxtaposing despair with hope. Techniques such as mindfulness and visualization serve as essential tools, fostering a sense of belonging amidst shared struggles in pain management.
How Can Caregivers Support Individuals With Chronic Pain?
Caregivers can support individuals with chronic pain through emotional support and effective communication strategies. By fostering connection and open dialogue, they help alleviate feelings of isolation, enhancing the individual’s overall well-being and sense of belonging.
What Are Common Misconceptions About Chronic Pain Psychology?
Chronic pain often resembles a storm, unpredictable and relentless. Many misconceptions, like equating pain with weakness, hinder pain management and emotional resilience. Understanding these myths fosters belonging and empathy, allowing for shared journeys toward healing and support.