Antidepressants are utilized in managing fibromyalgia symptoms, such as chronic pain and sleep disturbances. Different classes have varying effectiveness:
- Tricyclic Antidepressants (TCAs): Amitriptyline shows a 25-37% positive response rate.
- SNRIs: Duloxetine and milnacipran offer 30-37% of patients a 50% pain reduction.
- SSRIs: Show limited efficacy with a number needed to treat of about 10.
Long-term use requires careful monitoring and ongoing assessment of treatment efficacy. Further information on treatment options is available.
Key Takeaways
- Antidepressants, particularly SNRIs and TCAs, provide modest pain relief and improved quality of life for some fibromyalgia patients.
- Amitriptyline, a TCA, is effective in enhancing sleep quality and reducing pain at low doses.
- SNRIs, like duloxetine and milnacipran, show a positive response in 30% to 37% of patients for pain reduction.
- SSRIs offer mild pain relief but are generally less effective than SNRIs for fibromyalgia symptoms.
- Long-term effectiveness of antidepressants can vary, highlighting the need for tailored, multimodal treatment approaches.
Understanding Fibromyalgia and Its Symptoms
Fibromyalgia is a complex and chronic disorder characterized by widespread musculoskeletal pain. This condition primarily affects women and manifests as a constant dull ache lasting over three months, impacting both sides of the body.
Common Symptoms Include:
- Chronic pain in areas such as the neck, back, and limbs.
- Persistent fatigue, often described as flu-like exhaustion.
- Sleep disturbances, including insomnia and restless legs syndrome.
- Cognitive difficulties known as “fibro fog,” affecting memory and concentration.
- Increased sensitivity to sensory stimuli.
Although fibromyalgia has no known cure, effective symptom management is essential. Treatment strategies typically involve a combination of medications, exercise, and stress-reduction techniques, aiming to improve quality of life for those affected by this challenging condition.
Role of Antidepressants in Fibromyalgia Treatment

Antidepressants play a significant role in the management of fibromyalgia symptoms, particularly in addressing pain, sleep disturbances, and associated mood disorders.
- Meta-analyses indicate that antidepressants provide modest yet consistent benefits in reducing pain and improving health-related quality of life (HRQOL).
- While tricyclic antidepressants (TCAs) like amitriptyline show larger effect sizes, serotonin-norepinephrine reuptake inhibitors (SNRIs) such as duloxetine are FDA-approved and widely used.
- However, treatment challenges persist, as antidepressants demonstrate limited efficacy for fibromyalgia-related fatigue.
- Additionally, long-term use requires careful monitoring due to potential adverse effects.
Types of Antidepressants Used for Fibromyalgia

When managing fibromyalgia, various types of antidepressants have been identified as particularly beneficial for alleviating symptoms.
Antidepressant Classes
- Selective Serotonin Reuptake Inhibitors (SSRIs): Common options include fluoxetine, paroxetine, and sertraline. They enhance serotonin activity, providing mild pain relief but are less effective than SNRIs.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): FDA-approved medications like duloxetine and milnacipran address pain, fatigue, and mood issues.
- Tricyclic Antidepressants (TCAs): Amitriptyline is noted for its effectiveness in pain relief and sleep improvement.
Treatment Options
Both duloxetine and milnacipran are specifically FDA-approved for fibromyalgia, helping to rebalance altered pain signaling. Off-label use of SSRIs and SNRIs may also be considered, emphasizing the need for close monitoring.
Efficacy of Tricyclic Antidepressants (TCAs)

Tricyclic antidepressants (TCAs) have demonstrated significant efficacy in managing symptoms associated with fibromyalgia, particularly in pain reduction.
- Approximately 25% to 37% of fibromyalgia patients experience a notable clinical response to TCAs.
- Amitriptyline, a prominent TCA, is often highlighted for its effectiveness in alleviating pain and improving sleep quality at low doses (10-25 mg).
- The TCA mechanism involves inhibiting serotonin and norepinephrine reuptake, which is linked to pain modulation.
However, TCAs are associated with side effects, including dry mouth, sedation, and cardiovascular concerns, necessitating careful dosing. Despite these TCA side effects, their robust efficacy in reducing pain and enhancing overall health-related quality of life remains a compelling option in managing fibromyalgia symptoms.
The Impact of Selective Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)

The impact of selective serotonin-norepinephrine reuptake inhibitors (SNRIs) on fibromyalgia management is significant, particularly in pain reduction. Duloxetine and milnacipran are FDA-approved SNRIs specifically for this condition.
- Meta-analyses indicate that 30% to 37% of patients experience at least a 50% reduction in pain when using SNRIs, compared to 20%-24% on placebo.
- SNRIs utilize dual mechanisms by increasing serotonin and norepinephrine levels, effectively modulating pain pathways.
- Their analgesic effects involve activating descending pain inhibitory pathways, reducing overall pain perception.
- Long-term effectiveness and ideal dosing remain uncertain, necessitating further research.
The Limited Role of Selective Serotonin Reuptake Inhibitors (SSRIs)
Selective serotonin reuptake inhibitors (SSRIs) exhibit a limited role in the management of fibromyalgia, particularly regarding pain and fatigue relief.
- SSRIs show small to moderate effectiveness for pain reduction, with a Number Needed to Treat (NNT) of about 10.
- They outperform placebo in alleviating depressive symptoms, NNT of 13, yet do not greatly improve fatigue.
- Evidence indicates SSRIs’ limitations extend to sleep issues and physical functioning, remaining ineffective in those areas.
- Comparatively, SNRIs and tricyclic antidepressants demonstrate stronger efficacy for core fibromyalgia symptoms.
- The overall quality of evidence supporting SSRIs for fibromyalgia is low, characterized by small sample sizes and inconsistent outcomes.
Long-Term Considerations for Antidepressant Use
Long-term considerations for antidepressant use in fibromyalgia highlight significant gaps in understanding their sustained efficacy and impact on patient outcomes.
- Efficacy Limitations: Most studies focus on short-term results, with insufficient data on long-term effectiveness beyond 12 weeks.
- Patient Experiences: While antidepressants may improve pain, fatigue, and mood initially, these benefits often do not persist, raising questions about their long-term value.
- Long-Term Risks: Prolonged use can lead to side effects, including weight gain and withdrawal symptoms, which may affect adherence to treatment plans.
- Quality of Life: Extended antidepressant therapy does not guarantee improved health-related quality of life, emphasizing the need for thorough management strategies beyond medication alone.
Regular evaluation and adjustment of treatment regimens are essential to address these complexities.
Duloxetine: The FDA-Approved Option
Duloxetine, a serotonin-norepinephrine reuptake inhibitor (SNRI), stands as the first FDA-approved medication specifically indicated for the management of fibromyalgia. Approved in June 2008, duloxetine effectively reduces fibromyalgia-associated pain symptoms while also addressing chronic musculoskeletal pain.
Duloxetine Dosing:
- Starting dose: 30 mg per day.
- Titration: Increased to 60 mg per day based on tolerability and efficacy.
- Administration: Oral, typically once or twice daily.
Duloxetine Side Effects:
- Common side effects: Nausea, dry mouth, fatigue, constipation, dizziness.
- Most side effects diminish with continued use.
- Monitoring is essential for rare but serious effects.
Duloxetine supports long-term pain management, improving quality of life for fibromyalgia patients.
Future Directions and Research Gaps in Treatment
As the understanding of fibromyalgia evolves, significant gaps in research and treatment strategies become evident.
Research Gaps
- Ideal antidepressant dosages remain unclear, complicating personalized medicine approaches.
- Tailored dosing for accompanying symptoms like fatigue is underexplored.
- Long-term effects of different dosages in diverse populations lack sufficient data.
Diagnostic Challenges
- Evolving diagnostic criteria hinder targeted drug development.
- The role of neuroinflammation in treatment efficacy is inadequately studied.
Future Directions
- Personalized medicine could enhance responses through genetic and biochemical insights.
- Multimodal therapies integrating pharmacological and behavioral methods are being developed.
- Emerging treatments, such as TNX-102 SL, may improve existing antidepressant strategies, addressing multiple fibromyalgia mechanisms.
Frequently Asked Questions
How Do Lifestyle Changes Affect Fibromyalgia Symptoms Alongside Antidepressants?
Lifestyle changes, including dietary modifications and personalized exercise routines, greatly enhance fibromyalgia symptom management. These adjustments, when combined with medication, foster a sense of community and belonging among individuals traversing similar challenges and seeking improved well-being.
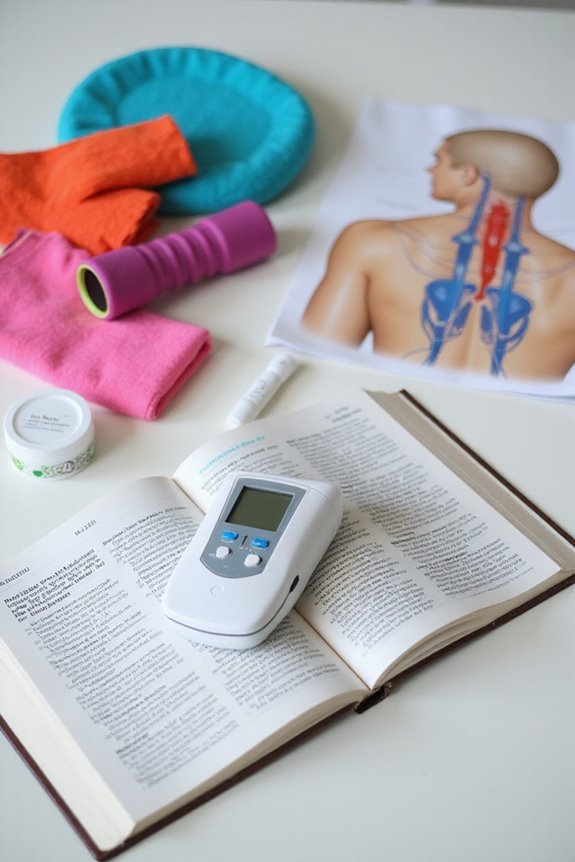
Are There Non-Pharmacological Treatments for Fibromyalgia?
In the intricate tapestry of fibromyalgia management, non-pharmacological treatments like mindfulness practices and physical therapy weave together to create a supportive community, fostering resilience and hope while alleviating symptoms through holistic approaches that nurture the mind and body.
What Are the Common Side Effects of Antidepressants for Fibromyalgia?
Common side effects of antidepressants for fibromyalgia include nausea, dizziness, and fatigue. Effective side effect management is essential, considering potential medication interactions. Patients often seek support to navigate these challenges and improve their treatment experience.
Can Antidepressants Be Combined With Other Fibromyalgia Medications?
“Two heads are better than one.” Combining medications in fibromyalgia treatment can enhance symptom relief through treatment synergy, allowing antidepressants to work alongside other therapeutics, fostering a thorough approach and improving overall patient well-being in a supportive community.
How Long Does It Take for Antidepressants to Show Effects on Fibromyalgia?
The treatment timeline for antidepressants typically reveals initial symptom relief within 2 to 4 weeks, although maximum benefits may take 8 to 12 weeks, emphasizing the importance of patience and consistent adherence for ideal outcomes.