Fibromyalgia pain results from multiple contributing factors, including:
- Neural Mechanisms: Central and peripheral sensitization heightens pain perception.
- Genetic Influences: Family history increases risk, with genetic variations affecting pain modulation.
- Environmental Triggers: Stressors, trauma, and climatic conditions can exacerbate symptoms.
- Autoimmune Factors: Immune dysregulation and autoantibodies may alter pain signaling pathways.
- Risk Factors: Higher incidence in women; often triggers include traumatic experiences. For a more thorough overview, additional details will be provided.
Key Takeaways
- Central sensitization amplifies pain signals in the CNS, lowering pain thresholds and increasing pain perception.
- Genetic predispositions, particularly in first-degree relatives, contribute to the likelihood of developing fibromyalgia.
- Environmental factors like stress, trauma, and climate changes can trigger and exacerbate pain symptoms.
- Autoimmune responses and neuroinflammation play a role in altering pain signaling and sensitivity.
- Emotional states and cognitive appraisal significantly influence the perception and severity of fibromyalgia pain.
Neural Mechanisms of Pain Sensitization
The neural mechanisms underlying pain sensitization in fibromyalgia represent a complex interplay of central and peripheral processes.
Central Sensitization
- Amplifies pain signals within the central nervous system (CNS), resulting in heightened pain perception.
- Structural and chemical changes in the CNS lead to reduced pain thresholds and hypersensitivity to stimuli.
Peripheral Sensitization
- Increases responsiveness of nociceptive nerve endings, sustaining central sensitization.
- Contributes to widespread pain distribution across the body.
Neurochemical Alterations
– Dysregulation of neurotransmitters, such as increased glutamate and decreased GABA, enhances pain transmission.
Cognitive-Emotional Sensitization
– Emotional states and cognitive appraisal can amplify pain perception.
Interpersonal Factors
– Social context and interactions influence pain sensitivity and coping mechanisms.
Genetic and Familial Influences

Genetic and familial influences considerably contribute to the risk of developing fibromyalgia, as evidenced by numerous studies indicating hereditary patterns within families.
- Familial patterns reveal that fibromyalgia often affects multiple family members, suggesting a genetic predisposition.
- The presence of a first-degree relative with the condition increases individual risk.
- Research highlights that this susceptibility is likely multifactorial, rather than attributed to a single gene.
- Genetic variations affecting neurotransmitter pathways play a role in pain modulation.
- Studies indicate that gene-environment interactions are significant, as environmental triggers may activate these genetic predispositions.
Understanding these genetic and familial influences can aid in developing targeted diagnostics and therapies, addressing the diverse needs of affected individuals.
Environmental Triggers and Stressors

Environmental triggers and stressors considerably influence the severity and onset of fibromyalgia symptoms. Key factors include:
- Climatic Influences: Low barometric pressure and high humidity can exacerbate pain. Cold and damp conditions lead to increased stiffness, while hot, humid weather may worsen fatigue.
- Chemical Sensitivities: Exposure to air pollutants and xenobiotics can heighten systemic inflammation and oxidative stress, intensifying fibromyalgia symptoms. Heavy metals and certain chemicals are particularly concerning.
- Electromagnetic Exposure: Electromagnetic fields may disrupt central nervous system functioning, impacting pain and cognitive symptoms.
- Trauma Effects: Both physical and emotional trauma are significant triggers. Chronic psychological stress influences symptom severity through neuroendocrine and immune dysregulation, complicating the fibromyalgia experience.
Autoimmune Contributions to Pain

Autoimmune mechanisms may play a critical role in the pathophysiology of fibromyalgia, influencing both symptom manifestation and severity.
- Autoantibodies impact pain sensitivity, leading to increased pain and muscle weakness.
- Immune dysregulation role is evident, as antibodies alter nerve function and pain signaling pathways.
- The presence of small nerve fiber loss is common among fibromyalgia patients, indicating immune-mediated changes.
- Research shows that injecting patient antibodies into animal models induces similar pain and lethargy symptoms.
- Neuroinflammation linked to immune activation contributes to widespread pain and tenderness.
- Acknowledging these autoimmune contributions may redefine fibromyalgia’s classification, paving the way for targeted immunomodulatory treatments and improved patient outcomes.
Continued exploration of these mechanisms is essential for advancing understanding and treatment approaches.
Risk Factors and Associated Conditions

What factors contribute to the development of fibromyalgia? Multiple risk factors have been identified, including:
- Genetic Predisposition: Family history increases risk.
- Gender: Women are affected twice as often as men.
- Age: Incidence peaks in middle age.
- Stressful Events: Traumatic experiences may trigger symptoms.
- Lifestyle Factors: Smoking and high body mass index are linked to increased risk.
Associated conditions include:
- Rheumatoid Arthritis and Lupus: These autoimmune diseases elevate the risk.
- Sleep Disorders: Frequently coexisting with fibromyalgia.
- Psychological Factors: Depression is commonly associated.
- Infectious Illnesses: Certain infections may trigger symptoms.
Lifestyle modifications, such as improved diet and physical activity, can also influence symptom management and overall health.
Frequently Asked Questions
Can Diet Affect Fibromyalgia Pain Symptoms?
Dietary changes can dramatically transform fibromyalgia pain symptoms, with individuals reporting relief through mindful food choices. Exploring food sensitivities further enhances this journey, fostering a sense of belonging among those seeking comfort and understanding in shared experiences.
How Is Fibromyalgia Diagnosed by Healthcare Professionals?
Healthcare professionals diagnose fibromyalgia through thorough symptom evaluation and adherence to established diagnostic criteria, focusing on widespread pain lasting over three months. This method emphasizes clinical judgment, often ruling out other conditions that mimic similar symptoms.
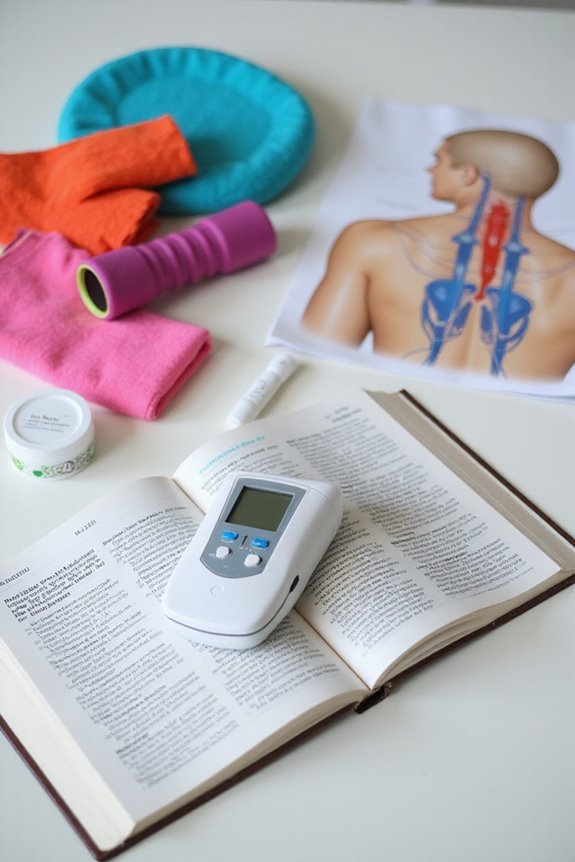
What Treatment Options Are Available for Fibromyalgia Pain?
Maneuvering the labyrinth of fibromyalgia treatments, patients explore medication management and alternative therapies. From pharmacological options like pregabalin to holistic practices like acupuncture, each path offers hope, fostering a sense of belonging in their healing journey.
Is Fibromyalgia Considered a Disability?
Fibromyalgia can qualify for disability benefits under specific fibromyalgia criteria. When symptoms markedly impair daily functioning and meet medical guidelines, individuals may receive support, acknowledging the challenges they face in the workplace and daily life.
Can Exercise Help Alleviate Fibromyalgia Pain?
Exercise, particularly low-impact activities and strength training, can alleviate fibromyalgia pain by improving muscle strength, enhancing sleep quality, and reducing stress. Many individuals find that regular movement greatly enhances their overall quality of life and well-being.