Chronic pain patients can use emergency departments (EDs) for acute pain episodes, but challenges exist. Pain management may suffer due to inconsistent evaluations and environmental factors. Staff skepticism about chronic pain can lead to misunderstandings, affecting trust. Opioid prescribing practices raise concerns regarding misuse, as nearly one-third of chronic pain patients receive opioids during visits. Coordination with primary care and using validated risk assessment tools enhances safety. Further insights into managing chronic pain in ED settings are beneficial.
Key Takeaways
- Chronic pain patients can safely use emergency rooms for acute pain episodes, but EDs are not designed for long-term pain management.
- Effective communication with ED staff is crucial, as misunderstandings about pain severity can affect treatment outcomes.
- Utilizing opioid risk assessment tools can enhance prescribing safety and minimize the risk of misuse during ED visits.
- Non-opioid analgesics should be prioritized, with opioids prescribed only as immediate-release formulations for short durations.
- Care coordination with primary care providers can improve treatment continuity and safety for chronic pain patients seeking emergency care.
Understanding the Role of Emergency Departments for Chronic Pain Patients
Understanding the role of emergency departments (EDs) for chronic pain patients is critical in addressing their unique healthcare needs.
- EDs often serve as the initial point of contact for individuals experiencing acute pain episodes related to chronic conditions.
- Emergency resources are sometimes limited, as these facilities are not designed for long-term pain management.
- Providers frequently resort to pain protocols that include opioid prescriptions, raising concerns about misuse.
- Utilizing opioid risk assessment tools can enhance safety in prescribing practices.
- Collaborative efforts among pharmacists and clinicians aim to tailor treatment based on pain severity and patient history.
Challenges in Pain Management Within the ED

Challenges in pain management within emergency departments (EDs) are multifaceted, impacting both patients and healthcare providers.
- Pain Evaluation Issues: Numeric Rating Scale (NRS) scores often lead to inconsistent morphine administration. Physicians may adjust these scores based on local protocols, contributing to treatment variability. Complementary tools, like the Behavioral Observation Scale 3 (BOS 3), are necessary for evaluating pain in non-verbal patients.
- Environmental Factors: Crowded and chaotic ED settings hinder effective pain management. Clinicians face rapid decision-making pressures, which may compromise thorough pain evaluations.
- Communication Gaps: Approximately 37% of patients report insufficient information regarding pain treatments. This lack of communication can negatively affect pain relief outcomes.
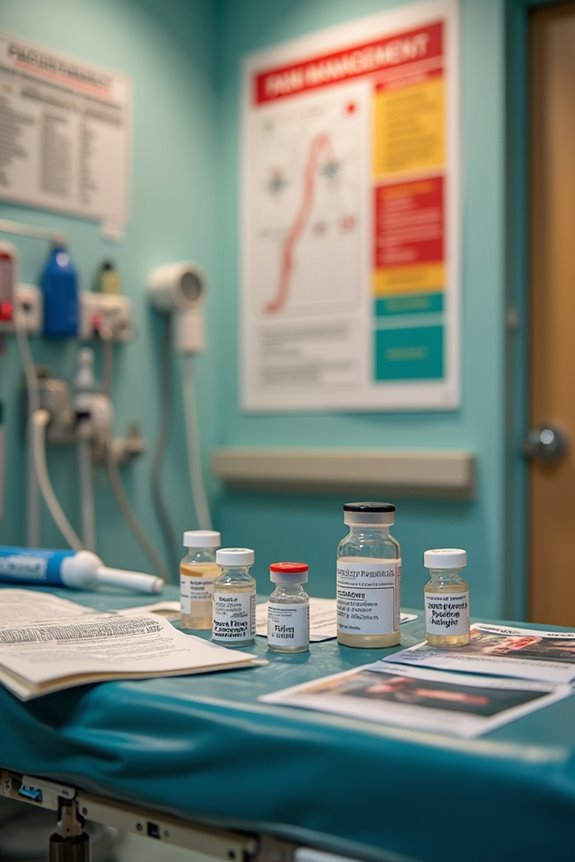
The Impact of Opioid Prescribing Practices

The impact of opioid prescribing practices in emergency departments (EDs) considerably affects the management of chronic pain patients.
- Nearly 43% of ED visits involve pain treatment, highlighting the significance of opioid regulations and prescribing guidelines.
- ED providers primarily focus on acute pain, avoiding long-acting opioids to minimize risks of dependency.
- During relevant visits, about one-third of chronic pain patients receive opioids, such as oxycodone and hydrocodone.
- Inadequate pain relief can lead to dose escalation and potential misuse, creating a tension between effective management and public health concerns.
- Prescribing frameworks emphasize evaluating pain relief adequacy and patient history to guarantee responsible opioid use while addressing chronic pain needs.
These practices ultimately influence continuity of care and patient outcomes in the ED setting.
Staff Attitudes and Patient Experiences in the ED

Staff attitudes toward chronic pain patients in the emergency department (ED) greatly influence the quality of care provided.
- Staff perceptions often lead to skepticism regarding chronic pain legitimacy, impacting care delivery.
- Negative biases may result in assumptions that patients are drug-seeking, which affects trust and communication.
- Communication barriers frequently arise, with patients feeling misunderstood and unable to convey pain severity effectively.
These factors contribute to strained patient-provider interactions, leading to emotional distress and dissatisfaction.
- Approximately 38% of high-frequency ED visitors present with chronic pain complaints, highlighting the significant presence of these patients.
- Improved provider training and enhanced communication strategies are essential to foster better patient experiences and outcomes in the ED.
Safety Considerations for Chronic Pain Patients Seeking Emergency Care

Safety considerations for chronic pain patients seeking emergency care are paramount in ensuring effective treatment and minimizing risks.
- Care Coordination: Assigning a care coordinator in the emergency department (ED) fosters continuity with primary care providers, enhancing communication and information sharing. This approach helps optimize pain management plans.
- Risk Assessment: Utilizing validated tools for opioid risk and pain severity assessments allows for appropriate treatment decisions.
- Pharmacological Safety: Non-opioid analgesics should be prioritized, with opioids prescribed only as immediate-release formulations and for short durations.
- Patient Education: Chronic pain patients must disclose recent procedures and understand the natural trajectory of their conditions to promote safe ED use.
Frequently Asked Questions
What Should Chronic Pain Patients Bring to an ED Visit?
Chronic pain patients should bring medical history, pain documentation, a list of medications, emergency contacts, and allergy information. These essentials guarantee effective communication and enhance care during an emergency department visit, fostering a sense of belonging.
How Can Patients Communicate Their Pain Effectively to ED Staff?
Effective communication in emergency departments involves using a pain scale to articulate pain levels clearly. Patients should prioritize their symptoms and engage openly, fostering understanding and cooperation with staff to achieve better care outcomes.
Are There Alternative Pain Management Options Besides Opioids in the ED?
In emergency departments, non-opioid therapies such as NSAIDs, acetaminophen, and ketamine provide alternative medications for pain management. These options, alongside multimodal approaches, enhance patient care while minimizing opioid dependency and maintaining satisfaction levels.
How Can Chronic Pain Patients Prepare for Potential Long Wait Times?
Chronic pain patients, facing agonizing waits, can adopt wait time strategies like bringing comfort items and entertainment. Employing pain management techniques such as mindfulness, they transform uncertainty into a more bearable experience, fostering a sense of belonging amidst discomfort.
What Follow-Up Care Should Chronic Pain Patients Seek After an ED Visit?
After an ED visit, chronic pain patients should prioritize follow-up appointments to reassess their condition. Implementing effective pain management strategies, including multidisciplinary approaches and medication adjustments, fosters a supportive environment for ideal recovery and well-being.