Long-term effects of using pain devices include:
- Efficacy: Spinal cord stimulation may diminish benefits after 1-2 years, while intrathecal drug delivery offers consistent relief.
- Complications: Risks involve infections, neurological issues, and device malfunctions.
- Quality of Life: Neuromodulation devices can improve mobility but may not guarantee functional enhancement.
- Maintenance: Rechargeable devices require regular charging; follow-up is essential for peak performance.
Further insights are available on device selection and management effectiveness.
Key Takeaways
- Long-term use of pain devices can improve functionality and quality of life, reducing reliance on medications for pain management.
- Efficacy of spinal cord stimulators may diminish after 1-2 years, highlighting the need for tailored device selection.
- Complications such as infections and device malfunctions can negatively impact long-term outcomes and functionality.
- Regular monitoring and maintenance of pain devices are crucial to ensure optimal performance and prevent complications.
- Neuromodulation devices can alleviate anxiety and depression associated with chronic pain, although individual results may vary.
Device Types and Their Functions
The landscape of pain management has evolved considerably with the introduction of various pain devices, each serving distinct functions tailored to patient needs.
Device Types and Their Functions
- Spinal Cord Stimulator (SCS) Systems: Sends low-level electrical pulses; includes conventional IPG, rechargeable IPG, and radiofrequency stimulator.
- Intrathecal Drug Delivery Systems: Also known as pain pumps; administer small medication doses directly into spinal fluid, customizable through programmable pumps.
- Radiofrequency Ablation Devices: Utilize radiofrequency energy to disrupt pain signals for longer-lasting relief, focusing on specific nerves or joints.
- Peripheral Nerve Stimulation (PNS) Devices: Deliver electrical stimulation to peripheral nerves, adjustable based on patient feedback.
- Transcutaneous Electrical Nerve Stimulation (TENS) Devices: Non-invasive, portable devices that provide electrical stimulation to alleviate pain at the skin level.
Each device selection aligns with specific patient pain management requirements, ensuring tailored treatment approaches.
Long-Term Efficacy of Pain Devices

Long-term efficacy of pain devices is a critical consideration in pain management, particularly as these technologies evolve. Effective device selection is essential to achieving desirable long-term outcomes.
- Studies indicate that buprenorphine transdermal patches provide sustained pain reduction over 36 months, with stable pain scores and minimal need for dose escalation.
- In contrast, spinal cord stimulation (SCS) may show diminishing benefits after 1-2 years, emphasizing the importance of understanding specific device capabilities.
- Long-term use of pain devices correlates with improved patient functionality and quality of life, reducing reliance on pharmacologic therapies and minimizing systemic side effects.
- However, variability exists among device types, necessitating careful consideration in selection to optimize long-term efficacy based on individual patient needs and conditions.
Potential Complications Associated With Devices
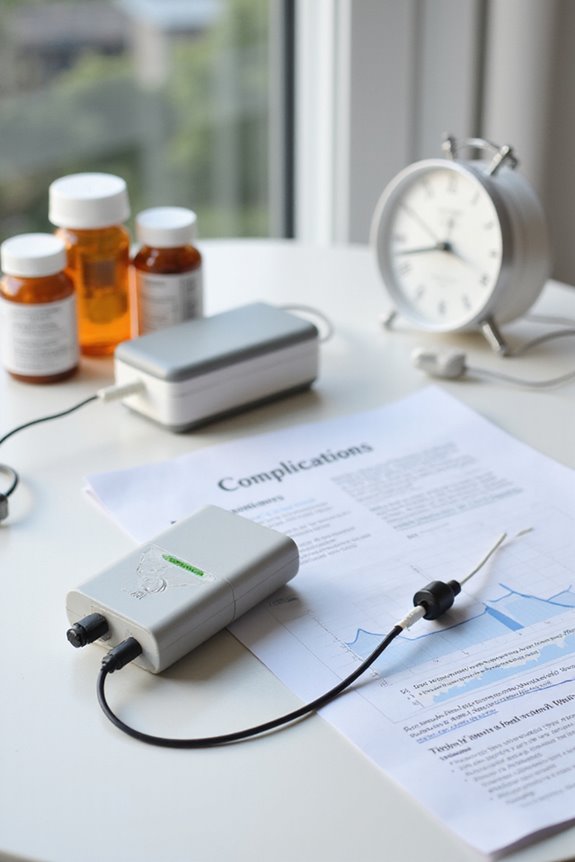
Potential complications associated with pain devices can greatly impact patient outcomes and overall satisfaction with treatment.
Infection Risks
- Infection at the implant site is common, potentially requiring removal or antibiotic therapy.
- Fluid collections, such as seromas, heighten infection risks and local discomfort.
Neurological Complications
- Dural puncture headaches may occur from accidental puncture during implantation.
- Serious injuries, including nerve root damage or spinal cord injury, can lead to permanent deficits like paralysis.
- Additional complications include erratic stimulation or device malfunction, necessitating further interventions.
Surgical Risks
- Procedures may result in spinal fluid leaks or excessive bleeding, complicating recovery.
- Each follow-up surgery increases cumulative risks, including infection and neurological damage.
Careful monitoring and adherence to post-operative guidelines are essential for minimizing these complications.
Impact on Quality of Life and Daily Functioning

Evaluating the impact of pain devices on quality of life and daily functioning reveals a complex interplay of outcomes.
- Functional Improvements: Neuromodulation devices can enhance mobility, allowing some patients to engage in daily activities previously hindered by pain. However, evidence on sustained improvement is inconsistent, with some individuals reporting negligible gains.
- Psychological Impacts: Successful pain management may alleviate anxiety and depression linked to chronic pain. Conversely, device management challenges can introduce stress and affect mental health.
- Complications: Device-related issues, such as infections or the need for additional surgeries, can impair functionality and diminish overall well-being. Additionally, TENS units offer a range of treatment options that may help users find a suitable approach for their specific pain needs.
Maintenance and Durability of Pain Devices
The maintenance and durability of pain devices are critical factors influencing their long-term effectiveness and patient satisfaction.
Battery Management
- Rechargeable devices require daily or weekly charging.
- Non-rechargeable batteries last several years but need surgical replacement.
- Regular clinical check-ups are essential for ideal battery replacement timing.
Device Monitoring
- Follow-up appointments assess performance and detect malfunctions early.
- Remote monitoring technology tracks device status and patient usage.
- Technical support includes software updates and troubleshooting.
Device Longevity
- Pain devices are designed for multi-year use but may need component replacements.
- Durable materials reduce risks of failure, although wear may occur over time.
- Awareness of potential hardware issues supports timely intervention and device longevity.
Cost Implications and Accessibility Issues
Cost implications associated with pain devices greatly impact patient access and overall healthcare expenditure.
- The average price for neuromodulation devices is approximately $16,940, with ongoing costs for devices like intrathecal pumps reaching about $792 monthly.
- High upfront costs and insurance variability create significant cost barriers, limiting accessibility for those without extensive coverage.
- Patients in lower socioeconomic brackets often face challenges in obtaining necessary devices.
- Geographic disparities further complicate access, particularly in rural areas with less healthcare infrastructure.
- Reimbursement policies are inconsistent, affecting eligibility and increasing out-of-pocket expenses.
- Despite these challenges, cost-effectiveness studies suggest that, in the long run, pain devices can reduce overall healthcare costs by minimizing additional medical care.
Frequently Asked Questions
Can Pain Devices Be Used for All Types of Chronic Pain?
Pain devices cannot be universally applied to all chronic pain types. Effective pain management often requires tailored approaches, considering the specific mechanisms and individual responses to treatment, fostering a sense of belonging in managing diverse pain experiences.
How Long Does the Implantation Procedure Typically Take?
Implantation duration typically ranges from 30 minutes to 3 hours, depending on surgical techniques and device complexity. Factors such as patient anatomy and prior surgeries can influence the overall time required for the procedure.
What Is the Recovery Time After Device Implantation?
The recovery timeline after device implantation typically spans 4 to 6 weeks, with individual experiences varying. Successfully maneuvering this period can enhance device longevity and foster a supportive environment for healing and improved pain management.
Are There Lifestyle Restrictions After Receiving a Pain Device?
After receiving a pain device, individuals face lifestyle adjustments akin to maneuvering a delicate dance; they must embrace activity limitations, carefully balancing movement and caution, ensuring safety while adapting to their new reality and maintaining connections with others.
How Can I Prepare for My First Appointment About Pain Devices?
To prepare for the initial appointment regarding device options, one should follow an appointment checklist that includes gathering medical records, tracking symptoms, formulating questions, and planning logistics to foster a supportive and informed treatment journey.





