Emergency settings utilize various pain treatments to provide effective relief. Key pharmacologic treatments include oral analgesics like acetaminophen and ibuprofen, injectable options such as morphine and fentanyl, and sub-dissociative ketamine. Routes for administration include intravenous (IV) for rapid relief, intranasal for quick access, and nerve blocks for targeted pain management. Non-pharmacologic techniques, like ice therapy and relaxation methods, further enhance treatment outcomes. Understanding these options and their applications leads to more informed pain management strategies.
Key Takeaways
- Oral analgesics like acetaminophen and ibuprofen are commonly used for mild to moderate pain relief in emergency settings.
- Injectable analgesics, including opioids and ketorolac, provide effective pain management for more severe cases.
- Intravenous administration offers rapid and titratable pain relief, ideal for acute situations.
- Non-pharmacologic therapies, such as ice therapy and relaxation techniques, can complement medications for overall pain management.
- Combined sedation approaches using low-dose propofol and analgesics improve patient comfort and procedural efficiency.
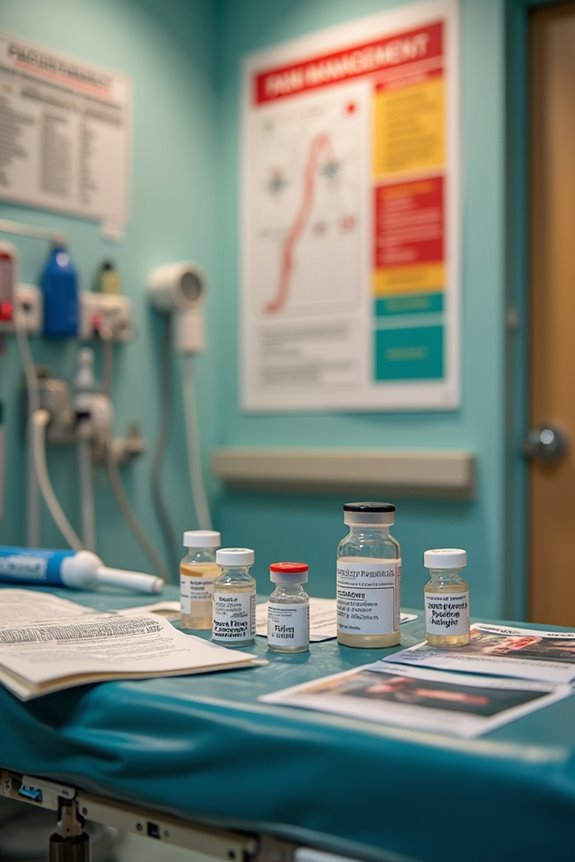
Pharmacologic Pain Treatments
Pharmacologic pain treatments in emergency settings play an essential role in the effective management of both mild and severe pain.
Oral Analgesics
- Acetaminophen: Effective for mild pain; minimal side effects.
- Ibuprofen: Commonly used oral NSAID; best gastrointestinal safety.
- Naproxen: Longer-lasting analgesia; superior cardiovascular profile.
- Combination Therapy: Acetaminophen with NSAIDs enhances efficacy for moderate pain.
Injectable Analgesics
- Ketorolac IV/IM: Effective for moderate pain when oral intake is unfeasible.
- Parenteral Opioids (Morphine, Fentanyl, Hydromorphone): For severe pain; requires monitoring.
- Sub-dissociative Ketamine (SDK): IV administration; may induce transient psychoperceptual effects.
These pharmacologic strategies guarantee tailored pain management in emergency situations, addressing patient needs effectively.
Routes of Analgesic Administration

Effective management of pain in emergency settings necessitates a thorough understanding of the various routes of analgesic administration.
Intravenous (IV) Advantages
- Rapid, titratable pain relief
- Quick onset critical for acute pain
- Preferred for opioid delivery
Intramuscular (IM) Disadvantages
- Severe injection site pain
- Unpredictable absorption
- Higher adverse effects compared to IV
Oral Limitations
- Slower onset and poor bioavailability
- Limited utility for immediate relief
Intranasal (IN) Benefits
- Non-invasive, rapid analgesia
- Useful when IV access is difficult
Subcutaneous Options
– Slower onset, but effective when IV is unavailable
Nerve Blocks
- Targeted analgesia with fewer systemic side effects
- Require clinician expertise for effective use
Sedative and Combined Analgesic-Sedation Approaches

In emergency settings, the management of pain often requires the incorporation of sedative and combined analgesic-sedation approaches to optimize patient outcomes.
Ketamine-Based Techniques
- Ketamine combined with low-dose propofol offers synergistic pain relief and sedation, minimizing respiratory depression risk.
- This combination provides effective analgesia while ensuring rapid recovery.
Propofol and Opioid Combinations
- Propofol, used with opioids like fentanyl, balances sedation and analgesia, facilitating procedures while promoting patient cooperation.
- Multimodal analgesia through low-dose propofol reduces the need for deep sedation.
Dexmedetomidine
– Dexmedetomidine supports sedation with analgesic-sparing effects, enhancing patient comfort and reducing delirium incidence.
These combined sedation techniques enhance pain management and procedural efficiency, ensuring better patient experiences in emergency care.
Non-Pharmacologic and Adjunctive Therapies

Non-pharmacologic and adjunctive therapies play a critical role in pain management within emergency settings, as they can complement pharmacological interventions and enhance patient comfort.
Ice Therapy: Cold packs can effectively reduce swelling and numb pain in acute injuries.
Manual Therapy: Techniques such as massage and spinal manipulation relieve muscle tension and alleviate back pain.
Movement Exercises: Low-impact activities like walking, stretching, and strengthening exercises help maintain mobility and improve flexibility, contributing to pain reduction.
Relaxation Techniques: Methods such as deep breathing, meditation, and yoga promote stress reduction and shift focus away from pain, fostering overall well-being.
These therapies are essential for creating a thorough pain management strategy, emphasizing both physical and psychological aspects of care in emergency situations.
Challenges and Considerations in Emergency Pain Management

Challenges in pain management within emergency settings are influenced by various factors that can hinder ideal patient care.
- Knowledge Deficits: A staggering 90% of healthcare providers in low- and middle-income countries report insufficient training in pain management, resulting in inadequate patient education.
- Operational Barriers: High patient volumes and time constraints limit thorough pain assessments, while communication barriers between staff and patients often lead to misunderstandings regarding pain management.
- Medication Accessibility: Scarcity of basic analgesics and inconsistent supply chains exacerbate untreated pain, complicating effective treatment options.
- Patient Perception: Nearly 37% of emergency patients feel they lack sufficient information about pain medications, indicating a critical need for improved communication to enhance satisfaction and outcomes.
These challenges collectively impede ideal pain management in emergency departments.
Specialized Pain Management Techniques
Specialized pain management techniques are crucial components in addressing acute pain within emergency settings. These methods include:
- Trigger Point Injections: Utilizing lidocaine or bupivacaine, these injections target acute myofascial pain, effectively reducing the need for systemic opioids.
- Epidural Steroids: Commonly used for spine and radicular pain, these injections decrease inflammation at nerve roots, providing relief for conditions like herniated discs.
- Osteopathic Manipulation: This non-pharmacological approach enhances musculoskeletal function and circulation, complementing medication-based treatments.
- Minimally Invasive Procedures: Techniques such as kyphoplasty offer immediate pain relief for vertebral fractures, making them crucial for patients with trauma-related pain.
These specialized techniques aim to optimize pain control while minimizing medication reliance, ensuring thorough patient care.
Frequently Asked Questions
How Is Pain Assessed in Emergency Settings?
Research indicates that 70% of emergency departments utilize pain scales for assessment. Pain assessment employs tools like the VAS and NRS to objectively measure pain intensity, enhancing understanding and management of patients’ experiences in critical situations.
What Are the Risks of Untreated Pain in Emergencies?
Untreated pain in emergencies poses significant consequences, including heightened chronic pain risk, impaired physical and mental health, and diminished quality of life. This cycle of suffering affects not only individuals but also their communities and social connections.
Can I Request a Specific Pain Treatment in the ED?
Patients can express preferences and request specific treatment options in the emergency department; however, these requests are evaluated based on clinical judgment, safety considerations, and adherence to established protocols, ensuring a balance between patient desires and medical necessity.
How Do Emergency Providers Prioritize Pain Management?
Emergency providers prioritize pain management strategies by employing various patient comfort measures. They emphasize early intervention, continuous assessment, and individualized treatment plans, fostering a supportive environment that reassures patients throughout their experience in the emergency department.
What Happens if My Pain Isn’t Relieved After Treatment?
When a patient, such as Jane, experiences unrelieved pain post-treatment, healthcare providers reassess pain management options, emphasizing follow-up care and ensuring appropriate referrals, fostering a supportive environment that encourages open communication about ongoing pain challenges.