Pain treatments vary globally due to disparities in access, cultural beliefs, and economic factors. High-income countries consume 69% of global opioids, whereas low-income nations have considerably lower availability, with morphine use differing by 5- to 63-fold. Sociocultural influences shape pain perceptions and treatment adherence. Non-pharmaceutical options, like traditional practices and psychological therapies, are frequently employed. Economic burdens of chronic pain can reach $635 billion annually in the U.S., underscoring the need for improved equity in pain management approaches. Further insights are available on this topic.
Key Takeaways
- Opioid availability drastically varies, with high-income countries consuming 69% of global resources compared to minimal use in LMICs.
- Cultural beliefs influence pain perception and treatment adherence, leading to diverse approaches to pain management across different societies.
- Non-pharmaceutical treatments like acupuncture and traditional practices are more prevalent in some regions, while pharmaceutical options dominate elsewhere.
- Economic factors, such as insurance policies and healthcare competition, significantly impact accessibility to pain management treatments among different countries.
- The global market for pain management drugs shows significant growth, with varying reliance on NSAIDs and opioids depending on local regulations and cultural attitudes.
Global Disparities in Pain Treatment Access
Global disparities in pain treatment access present significant challenges, particularly for low- and middle-income countries (LMICs). These nations, which comprise 85% of the global population, face profound pain management disparities, especially regarding opioid availability.
Key statistics include:
- High-income countries consume 69% of global opioid resources.
- The WHO notes a 5- to 63-fold difference in morphine consumption between high-income and low-income countries.
- Opioid use in Africa and South America represents less than 0.1% of North American levels.
Economic barriers, such as high medicine costs and restrictive regulations, further exacerbate global healthcare inequalities. Additionally, inadequate education among healthcare providers limits effective pain management. Addressing these disparities is critical for improving health outcomes in underserved populations.
Sociocultural Influences on Pain Perception

Sociocultural influences greatly shape pain perception, which is critical to understanding disparities in pain management globally.
- Cultural beliefs dictate interpretations of pain, often viewing it as a natural part of life or a test of endurance.
- Attitudes toward pain expression vary; some cultures promote openness, while others value stoicism, affecting pain reporting.
- Pain sensitivity and tolerance levels differ widely across cultures, influenced by social norms.
- Cultural narratives guide coping mechanisms and management strategies, frequently incorporating traditional practices.
- Social roles impact pain expression, with gender expectations dictating how pain is shown.
These factors create barriers in pain assessment, potentially leading to miscommunication and affecting treatment adherence and outcomes. Understanding these influences is essential for effective pain management.
Pharmaceutical Approaches to Pain Management
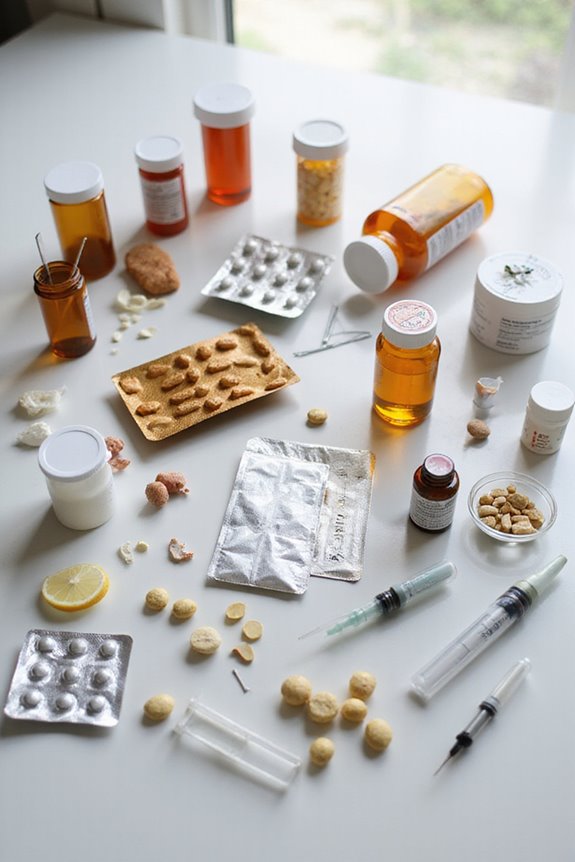
Pharmaceutical approaches to pain management are diverse, reflecting variations in market dynamics, drug classes, and regional access.
- The global market for pain management drugs is projected to grow from $84.6 billion in 2023 to $109.9 billion by 2028.
- Non-steroidal anti-inflammatory drugs (NSAIDs) represent approximately 24.1% of the market, favored for their affordability and accessibility.
- Opioids, while essential for severe pain, face strict opioid regulations that affect their availability, especially in North America and Europe.
- In developing regions, retail pharmacies often serve as primary access points due to limited healthcare infrastructure.
- Drug availability varies markedly, influenced by local regulations, cultural attitudes, and healthcare systems, leading to different therapeutic strategies worldwide.
Non-Pharmaceutical Treatment Options

What options exist beyond pharmaceuticals for managing pain? Various non-pharmaceutical treatments provide effective alternatives:
- Acupuncture Benefits: Commonly practiced in East Asia, this technique balances essential energy and is gaining global recognition.
- Yoga Effectiveness: Utilized worldwide, yoga combines physical postures and breathing to alleviate chronic pain.
- Cultural Therapies: Indigenous practices, such as traditional massage, offer tailored approaches based on local beliefs.
- Physical Modalities: Techniques like physical therapy, hydrotherapy, and electrical stimulation are employed globally to enhance movement and reduce pain.
- Psychological Approaches: Mindfulness techniques, cognitive-behavioral therapy, and support groups address the emotional aspects of chronic pain.
These diverse options reflect a growing understanding of holistic pain management in various healthcare systems.
Economic Factors Impacting Pain Care

Economic factors markedly influence pain care across various healthcare systems. The economic burden of chronic pain can reach up to $635 billion annually in the U.S., highlighting the need for effective management strategies.
- Insurance Reimbursement: Variations in insurance reimbursement policies can affect treatment accessibility. Providers may prioritize treatments that are reimbursed, potentially limiting patient options.
- Market Competition: Increased competition among healthcare providers often leads to a broader range of treatment options. This competition can also contribute to lower costs, benefiting consumers.
- Healthcare Expenditures: Rising expenditures, particularly in spine-related care, reflect the growing economic impact of chronic pain.
Addressing these economic factors is essential for improving pain management outcomes across diverse populations.
The Role of Technology in Pain Management
Technological advancements are reshaping the landscape of pain management, offering innovative solutions that enhance treatment efficacy and patient engagement.
- Virtual Reality (VR) is utilized for immersive distraction techniques, effectively reducing pain perception during treatments and rehabilitation.
- Artificial Intelligence (AI) and machine learning analyze individual pain patterns, allowing for personalized and optimized treatment plans.
- Wearable technologies enable continuous pain monitoring and real-time physiological data collection, tailoring therapies to individual needs.
- The global pain management devices market is projected to grow at a CAGR of 6.6% to 8.4% from 2024 to 2035, indicating rising demand for tech-based solutions.
- Digital therapeutics and telehealth improve accessibility, addressing geographic barriers and enhancing patient empowerment in pain management.
Strategies for Addressing Inequities in Pain Treatment
How can healthcare systems effectively address inequities in pain treatment across diverse populations?
To mitigate disparities, several strategies can be implemented:
- Community Interventions: Initiatives such as Essential Health Packs (EHPs) can deliver essential pain medications to underserved areas in low- and middle-income countries (LMICs), addressing direct access issues.
- Advocacy Initiatives: Organizations advocating for policy reform can promote balanced regulations that facilitate opioid access while ensuring safe usage, particularly in regions with strict controls.
- Education and Training: Enhancing the education of healthcare providers on pain management can improve treatment outcomes, especially within marginalized communities affected by chronic pain.
Addressing these areas is vital for creating equitable pain treatment frameworks that cater to the diverse needs of populations globally.
Frequently Asked Questions
How Do Cultural Beliefs Affect Pain Treatment Choices in Different Countries?
Cultural perceptions greatly influence treatment preferences, shaping how individuals interpret pain and select therapies. Varied beliefs regarding pain management lead to diverse approaches, with some favoring traditional remedies while others lean towards conventional medical practices.
What Role Do Healthcare Professionals Play in Pain Management Variations?
In the intricate tapestry of pain management, healthcare professionals weave their expertise through training and collaboration. Their collective knowledge and support shape treatment approaches, nurturing a community where effective pain relief becomes a shared journey toward healing.
How Is Pain Treatment Education Conducted in Low-Income Countries?
Pain education in low-income countries emphasizes multidisciplinary approaches and tailored curricula to improve healthcare access. Initiatives aim to equip providers with essential skills, addressing significant gaps in pain management and fostering better patient outcomes in resource-limited settings.
Are There Specific Regulations Governing Pain Medications in Various Countries?
“An ounce of prevention is worth a pound of cure.” Regulatory frameworks governing medication approval differ greatly, with some countries prioritizing access and safety, while others impose stringent controls, shaping patient experiences and treatment outcomes globally.
How Do Patient Rights Influence Access to Pain Treatments Globally?
Patient rights greatly influence access to pain treatments globally, with legal frameworks often determining the extent of patient autonomy. Stronger protections can foster equitable access, ensuring that all individuals receive necessary pain relief and management.