To prepare an emergency plan for pain crises, it is essential to:
- Conduct thorough pain assessments using validated tools.
- Utilize pharmacological strategies, including immediate-release opioids and non-opioid analgesics.
- Implement non-pharmacological methods, such as mindfulness and TENS therapy.
- Adhere to emergency department protocols for managing acute pain effectively.
- Guarantee personalized discharge planning that addresses the specific needs of vulnerable populations.
This all-encompassing approach enhances management strategies and improves patient outcomes. Further insights can be obtained from continued exploration.
Key Takeaways
- Identify and document specific pain triggers, symptoms, and individual pain management preferences in the emergency plan.
- Include a list of prescribed medications, dosages, and instructions for managing pain during a crisis.
- Establish clear communication channels with healthcare providers for rapid access to pain management resources.
- Create a support system involving family or caregivers who can assist during pain crises and understand the emergency plan.
- Schedule regular reviews and updates of the emergency plan to ensure its effectiveness and alignment with current health status.
Understanding Pain Crises: Assessment and Identification
How can healthcare providers effectively assess and identify a pain crisis?
Pain Assessment
Healthcare providers should conduct a focused history, asking targeted questions about pain onset, location, and progression. Pain evaluation tools such as the 0–10 scale or visual analog scales can provide quantifiable data.
Crisis Identification
Identification of a pain crisis involves recognizing severe, uncontrolled pain, often rated 7/10 or higher, that develops rapidly and causes significant distress. Symptoms may include acute pain, anxiety, and physical signs like sweating and restlessness.
Importance of Prompt Identification
Rapid recognition is vital; it reduces suffering, facilitates timely management, prevents complications, and invokes necessary resources. Documentation by a second caregiver can enhance accuracy and support future interventions, ensuring thorough care for affected patients.
Pharmacological Approaches for Effective Pain Management

Effective pain management during crises relies on a combination of pharmacological approaches tailored to the patient’s specific needs.
First-Line Analgesics
- Acetaminophen and NSAIDs are primary agents for mild to moderate pain.
- NSAIDs inhibit cyclooxygenase enzymes, reducing inflammation and pain.
- Acetaminophen is versatile, available orally, rectally, or intravenously.
Opioid Alternatives
- Opioids offer short-term improvements but carry risks of tolerance and dependence.
- Long-term use lacks strong evidence for sustained relief and can exacerbate pain.
Adjuvant Medications
- Antidepressants and antiepileptics can enhance pain management.
- Local anesthetics provide targeted relief for specific pain types.
Multimodal Strategies
- Combining analgesic combinations optimizes pain relief while minimizing opioid reliance.
- Regional nerve blocks can be effective adjuncts in complex pain scenarios.
Integrating Non-Pharmacological Strategies

Integrating non-pharmacological strategies into pain management plans enhances overall effectiveness and patient outcomes. These approaches can markedly improve the quality of life for individuals experiencing pain.
Mindfulness Techniques:
- Mindfulness-based stress reduction (MBSR) meditation aids in pain reduction and promotes adherence.
- Progressive muscle relaxation regulates muscle tension and stress-related pain.
Cognitive Strategies:
- Cognitive-behavioral therapy (CBT) reshapes pain perception, empowering chronic pain self-management.
- Hypnotherapy utilizes guided relaxation to alter pain perception effectively.
Complementary Practices:
- Acupuncture stimulates endorphin release, serving as a first-line treatment for certain pain types.
- Yoga and Tai Chi combine gentle movement with mindfulness, reducing chronic pain.
Additionally, incorporating TENS therapy can provide drug-free pain relief, making it a valuable tool in a comprehensive pain management strategy.
These strategies foster a thorough approach to pain management, underscoring the importance of holistic care.
Pain Management Protocols in Emergency Departments

Pain management protocols in emergency departments play a critical role in addressing acute pain effectively. These protocols guide clinicians in selecting appropriate interventions, utilizing both pharmacological and non-pharmacological methods tailored to individual patient needs and pain severity.
Key components of emergency protocols include:
- Immediate-release opioids as a primary choice for severe pain, prescribed at minimal effective doses.
- Utilization of non-opioid analgesics, such as NSAIDs and acetaminophen, to reduce opioid reliance.
- Thorough assessment of pain characteristics, documented to inform treatment choices.
- Regular reassessments to guarantee effective pain relief and safety, particularly in special populations.
Essential Components of Discharge Planning

Discharge planning is an essential process that guarantees patients move safely from the hospital to their home environment. Key components include:
- Assessment Upon Admission: Evaluating medical status, home environment, and support systems while identifying barriers to recovery.
- Personalized Plan Development: Crafting individualized care plans that include medication prescriptions, follow-up appointments, and lifestyle modifications based on patient preferences.
- Patient and Caregiver Education: Providing clear discharge instructions, medication guidance, and technical care demonstrations to enhance understanding.
- Coordination With Providers: Ensuring seamless communication among healthcare providers and arranging necessary community resources.
- Follow-Up and Ongoing Evaluation: Scheduling post-discharge check-ins to monitor adherence and address emerging issues.
These essential elements enhance discharge readiness factors, ensuring thorough support for patients moving home.
Special Considerations for Vulnerable Patient Populations
Addressing the unique needs of vulnerable patient populations is crucial in the domain of pain management, particularly as these groups often experience higher rates of chronic pain and associated challenges.
Key considerations include:
- Higher Prevalence: Vulnerable populations, such as low-income individuals and those with chronic diseases, show increased rates of high-impact chronic pain.
- Access Barriers: Economic constraints and geographic isolation limit access to pain management resources, particularly in rural areas.
- Specialized Care Needs: Patients with cognitive impairments, like dementia, require tailored assessment tools to address their pain effectively.
- Coordinated Care: Multidisciplinary approaches are essential for managing complex cases, ensuring that pain specialists, rehabilitation, and social support are integrated.
Recognizing these factors is crucial for improving pain management outcomes within vulnerable populations.
Resources for Ongoing Pain Management and Support
Access to appropriate resources for ongoing pain management and support is essential for individuals, especially those in vulnerable populations. Key components include:
- Support Resources: Access to support groups and peer networks offers emotional and practical coping strategies. These connections foster a sense of belonging.
- Pain Education: Patient education programs enhance self-management skills, empowering individuals to maneuver their pain effectively.
- Multidisciplinary Approaches: The integration of physical therapy, cognitive behavioral therapy, and complementary therapies provides thorough care.
- Telehealth Services: Online resources expand access, particularly for those in rural or mobility-limited areas.
- Case Management: Social workers assist in maneuvering insurance and disability services, ensuring thorough support.
Utilizing these resources can greatly improve the quality of life for those managing chronic pain. Additionally, incorporating topical pain relief gels into pain management strategies can provide targeted relief and enhance overall comfort.
Frequently Asked Questions
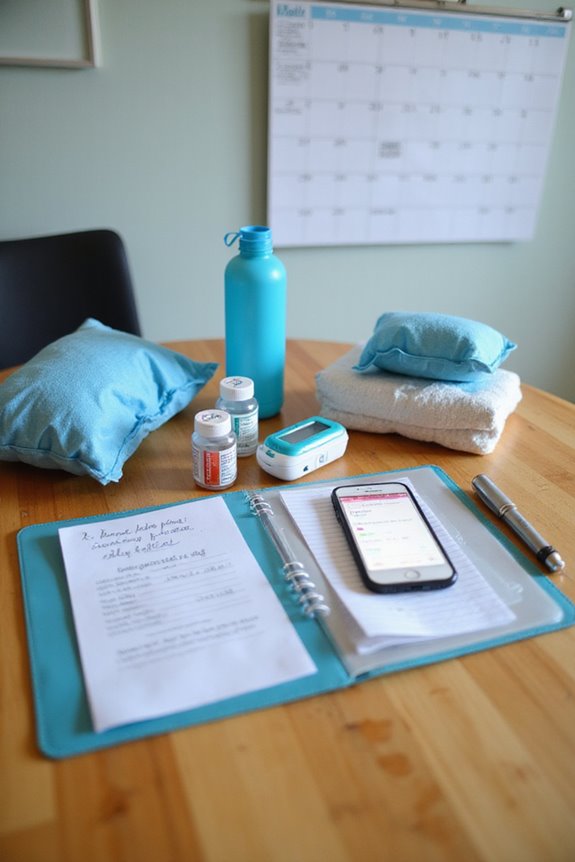
What Should I Include in My Emergency Pain Management Kit?
When considering an emergency pain management kit, essential medication options include ibuprofen and acetaminophen. Additionally, kit essentials should encompass antiseptic wipes, adhesive bandages, and antihistamines, fostering a sense of preparedness and community support.
How Can I Communicate My Pain Needs to Healthcare Providers?
Effective communication of pain needs involves using precise pain vocabulary to articulate experiences clearly. This fosters understanding and trust between patients and providers, enhancing collaborative dialogue and ensuring appropriate pain management strategies are established and maintained.
Are There Specific Warning Signs for Worsening Pain Crises?
Like storm clouds gathering on the horizon, specific warning signs for worsening pain crises emerge through symptom tracking. Pain triggers, such as dehydration or stress, can escalate discomfort, prompting the need for immediate attention and care.
What Lifestyle Changes Can Help Prevent Pain Crises?
Lifestyle changes to prevent pain crises include effective stress management techniques and dietary adjustments. Adopting anti-inflammatory foods alongside mindfulness practices fosters a supportive environment for well-being, enhancing resilience and promoting a sense of community among individuals.
How Can Family Members Support Someone Experiencing a Pain Crisis?
In the tempest of pain, family members become anchors, offering steadfast emotional support and guiding pain management together. Their collective strength fosters resilience, transforming the experience into a shared journey, reducing isolation and nurturing belonging amidst adversity.