Researchers measure pain in clinical studies using several methods, including:
- Self-Report Scales: Numeric Rating Scales (NRS), Visual Analog Scales (VAS), and Verbal Rating Scales (VRS) assess pain intensity.
- Observational Tools: FLACC and COMFORT scales evaluate pain in non-verbal patients.
- Quantitative Sensory Testing: Measures thresholds and responses to stimuli.
These approaches align with IMMPACT core domains, ensuring thorough assessment. Each method offers distinct advantages, influencing treatment evaluation methods. Further details are available in the subsequent sections.
Key Takeaways
- Researchers utilize self-report scales like NRS and VAS to assess pain intensity from the patient’s perspective.
- Observational tools like the FLACC scale are employed for non-verbal patients to evaluate pain levels.
- Quantitative Sensory Testing (QST) measures pain thresholds and responses using calibrated stimuli for a more objective assessment.
- Clinical Outcome Assessments (COAs) are crucial for evaluating treatment efficacy, incorporating patient-reported outcomes and clinician-reported outcomes.
- Electronic Data Capture (EDC) methods enhance data quality and timeliness, allowing for real-time pain assessment through digital platforms.
Pain Measurement Methods
Pain measurement methods are essential tools in clinical studies, as they provide insights into patient experiences and treatment effectiveness. Various approaches exist for pain assessment, each with unique strengths and measurement challenges.
Self-Report Scales
- Numerical Rating Scale (NRS): 0-10 or 0-100 scale for pain intensity.
- Visual Analog Scale (VAS): Continuous line for patients to mark pain levels.
- Faces Pain Scale Revised (FPS-R): Uses facial expressions, ideal for children or cognitively impaired.
Observational Tools
- FLACC scale: Rates pain based on observable behaviors in non-verbal patients.
- COMFORT Pain Scale: Measures distress in critical care settings.
Quantitative Sensory Testing (QST)
– Employs calibrated stimuli to assess pain thresholds and responses, aiding in tailored treatment strategies.
These diverse methods enhance the understanding of pain but may present challenges in consistent application across patient populations.
IMMPACT Core Domains for Pain Assessment

Effective assessment of chronic pain relies on standardized frameworks, such as the IMMPACT Core Outcome Domains. These domains encompass six critical areas essential for chronic pain clinical trials:
- Pain: Focuses on intensity and quality, measured through validated scales.
- Physical Functioning: Evaluates daily activities impacted by pain.
- Emotional Functioning: Addresses mood disorders like depression and anxiety.
- Participant Ratings of Improvement and Satisfaction: Captures patients’ perceptions of treatment efficacy.
- Symptoms and Adverse Events: Monitors treatment-related side effects.
- Participant Disposition: Assesses retention and completion rates.
The IMMPACT domains facilitate data comparison, enhance outcome reporting, and streamline clinical decision-making, ultimately contributing to evidence-based treatment approaches in chronic pain management.
Clinical Outcome Assessments and Regulatory Recommendations

Clinical outcome assessments (COAs) play an essential role in evaluating treatment efficacy in chronic pain clinical trials. These assessments include various types, such as patient-reported outcomes and clinician-reported outcomes, each critical for understanding patient experiences.
Regulatory bodies like the FDA and EMA emphasize the necessity of assessment validity and clinical significance in COA selection. Their guidelines advocate for COAs demonstrating robust psychometric properties and relevance to patients.
Key recommendations include:
- Use of patient-reported outcome measures (PROMs) to assess pain intensity and functional impact.
- Methodologic justification for COAs in regulatory submissions.
- Ongoing research to enhance COA precision and interpretability.
Such standards guarantee that COAs provide meaningful insights into treatment effectiveness, facilitating informed regulatory decision-making.
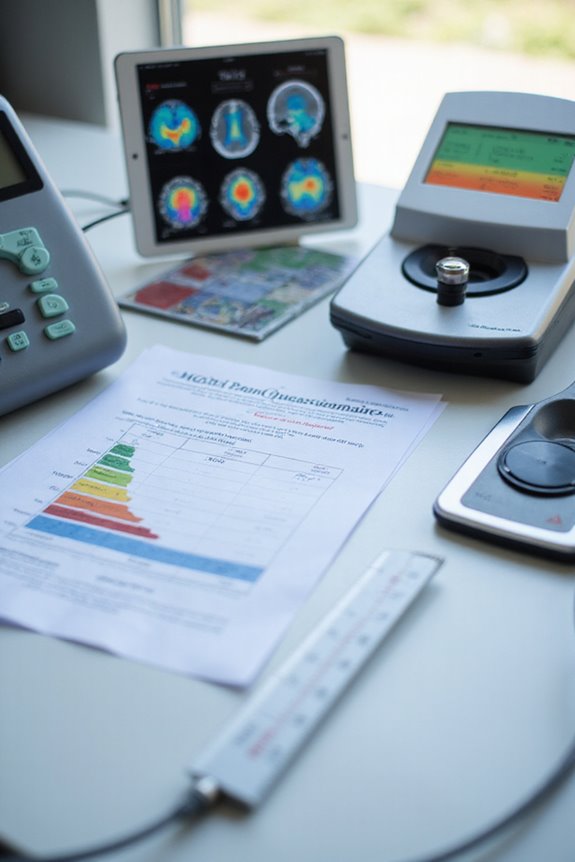
Data Capture and Assessment Modalities

In the evaluation of treatment efficacy, the selection of appropriate data capture and assessment modalities is paramount.
Electronic Data Capture Methods
- Electronic data capture (EDC) employs tools like digital diaries, smartphones, and web-based platforms for pain assessment.
- Studies reveal a high congruence (correlation coefficient ~0.92) between electronic and conventional methods.
- EDC enhances data completeness and timeliness, with patients favoring its convenience.
Sensor Integration
- Physiological and environmental sensors enable passive collection of pain-related biological signals.
- This integration allows real-time data analysis within patients’ environments, reducing reporting burdens.
- Combining sensor data with patient-reported outcomes offers a thorough view of pain dynamics.
These modalities collectively support improved data quality and more effective clinical trials.
Standardized Pain Measurement Instruments
Standardized pain measurement instruments serve as essential tools in the assessment of pain across various clinical settings. These instruments provide reliable methods for subjective reporting, enabling comparability in pain scale comparisons.
Common Scales:
- Numerical Rating Scale (NRS): Rates pain from 0 (no pain) to 10 (worst pain).
- Visual Analog Scale (VAS): Allows patients to mark pain intensity on a continuous line.
- Verbal Rating Scales (VRS): Utilizes descriptors such as “none” and “severe.”
Multidimensional Tools:
- McGill Pain Questionnaire (MPQ): Evaluates sensory and affective aspects of pain.
- Brief Pain Inventory (BPI): Assesses severity and impact on daily activities.
These standardized instruments enhance clarity in measuring pain, fostering a shared understanding among healthcare providers and patients.
Frequently Asked Questions
What Factors Influence Patients’ Pain Reporting Accuracy?
Numerous factors influence patients’ pain reporting accuracy, including emotional factors that affect pain communication. Anxiety, depression, and cultural backgrounds shape perceptions, while cognitive impairments and clinical settings further complicate effective expression of pain experiences.
How Do Cultural Differences Affect Pain Assessment?
Cultural norms profoundly shape communication styles regarding pain, influencing how individuals express or suppress discomfort. These variations can lead to misunderstandings in clinical settings, ultimately affecting pain assessment and the effectiveness of treatment strategies.
Are There Specific Populations With Unique Pain Measurement Needs?
Certain populations, like pediatric populations and elderly patients, exhibit unique pain measurement needs. Their developmental stages and cognitive impairments necessitate tailored assessment tools, ensuring accurate pain evaluation and fostering a sense of understanding and support in care.
How Does Pain Perception Change Over Time?
As the saying goes, “Time heals all wounds,” yet pain progression often deepens with age. Emotional factors intricately intertwine with pain perception, illustrating a complex journey that evolves, shaping individuals’ experiences and connections throughout their lives.
What Role Do Placebo Effects Play in Pain Trials?
Placebo effects considerably influence pain trials, driven by placebo mechanisms and patient pain expectations. These effects can enhance perceived pain relief, complicating the assessment of true drug efficacy and highlighting the intricate relationship between perception and treatment outcomes.